By Mike Darwin
Introduction
A short while ago, these remarks were posted in the comments section of Chronosphere: “I’ve often heard it said that case reports have been very inconsistent. I’ve read a haphazard sampling of Alcor case reports. They are in different styles with differing levels of information. I recommend you take a look at some of the case reports from different eras in addition to the ones you’ve already seen.” I have also been asked, on Cryonet, to comment on case reports in cryonics. After some reflection, I realized that I’ve been doing this, one way or another, for nearly 40 years now – arguably since “Perfusion and Freezing of a 60 Year Old Woman” was published in 1973 – which, while a case report, was also an indictment of cryonics stabilization and cryoprotective perfusion practice at that time.[1] Clearly, that approach has not worked, and so I’ve decided to take a different tack, principally laying out the basis for evaluating case reports in such a way that any diligent layman or medical professional can do it themselves.
 Figure 1: Aschwin deWolf
Figure 1: Aschwin deWolf
Aschwin de Wolf has written an excellent article discussing the importance of case reports in cryonics and has listed four key reasons case reports should be published:
1. To provide a transparent and detailed description of procedures and techniques for members of the cryonics organization and the general public.
2. To validate current protocol and procedures in general, and its actual implementation in particular.
3. To serve as a medical record to assist with future attempts to revive the patient.
4. To gain more scientific credibility.[2]
Aschwin’s article is the primer to this one, and I recommend that it be read as an essential adjunct to this one. In particular, at the end of his article he notes the need:
“To establish a template for…case reports the following approach can be followed. First, it is established what kind of information is essential for doing a meta-analysis of all cryonics cases. Then these parameters are reverse-engineered to create a template for writing case reports that reconcile the need for economy of expression and documenting all the relevant aspects of a case. One important advantage of producing such case reports is they permit easier consultation of the technical details of the case and still meet the fundamental objectives of writing case reports.
The history of case report writing in cryonics shows an erratic potpourri of approaches and styles. One of the most unfortunate victims has been the objective of using case reports to improve the practice of human cryopreservation and to formulate meaningful research questions for the sciences that inform cryonics. But if systematic thought is given to the objectives of case reporting outlined in this document, steps can be taken to leave this unsatisfactory situation behind while meeting the needs of a growing cryonics organization.”
In this he is correct, for while Jerry Leaf and I used a fairly consistent approach to case reporting and presentation of all of the available data, this has not been the case elsewhere in cryonics. A more serious problem is that even the best written cryonics case reports are largely opaque to almost all readers, including those with considerable medical knowledge; and what’s worse, poorly written case reports can be downright misleading – even if they contain all the necessary information required to draw the correct conclusions about the quality of care the patient received. The goal of this series of articles is to equip the reader with the tools necessary to make an accurate assessment of the quality of care cryonics patients, both individually and as a group, are receiving from their respective cryonics organizations.
The Problems of Narrative and Context
 Figure 2: How meaningful is pulse oximetry in the context of evaluating the efficacy of cryopatient Stabilization?
Figure 2: How meaningful is pulse oximetry in the context of evaluating the efficacy of cryopatient Stabilization?
Broadly speaking, there are two obstacles to making sense of case reports. First it is necessary to establish the critical elements that must be present in the case report and to explain what they are and what they mean; and to do so in the context of cryonics. As an example, pulse oximetry a modality frequently used to evaluate the effectiveness of cardiopulmonary support (CPS) during cryopatient Stabilization is now a commonly understood physiological parameter, since it is used in a wide array of sports performance monitoring devices, and has arguably become (along with heart rate (pulse), respiration rate, blood pressure and temperature) the 5th Vital Sign in medicine.[3, 4] Most people understand, at a minimum, what the number generated by the pulse oximeter, and displayed under the heading SpO2 represents: the percentage of blood oxygen saturation ranging from 0 to 100%. It isn’t terribly important that they understand the nuances (i.e., the SpO2 is the mixed arterial and venous oxygen saturation; some of the signal comes from the venous blood, and thus the number displayed does not represent an accurate measure of the arterial blood oxygen saturation) for the SpO2 to be of value in everyday life, or even in medicine, most of the time.
However, it is important that readers, lay and medically sophisticated alike; understand the limits of SpO2 measurement in the context of cryonics Stabilization and Transport. During the agonal process many cryopatients will be in a state of profound shock for many hours prior to cardiac arrest. During this interval of depressed blood pressure and perfusion, the body attempts to maintain blood circulation to the vital organs at the expense of the peripheral tissues by reducing, or even eliminating flow to the skin and appendages; hence the dusky or even frankly gray pallor associated with shock, as well the cooling of the extremities. Most pulse oximeters are not designed to accurately read blood oxygen saturations below 70-80%, thus, depending upon the type of device being used, SpO2 readings for much of the agonal period, and in most cases much or all of the post-cardiac arrest cardiopulmonary support period, may be nothing more than meaningless numbers produced by a pulse oximeter that is in reality functioning as random number generator.[5-7]
In some patients, the agonal vasoconstriction may be so severe and so long lasting that there is simply no measureable pulse to detect in the peripheral tissues. In other words, perfusion has ceased altogether and may not return, even if an adequate blood pressure is subsequently generated by closed chest cardiopulmonary or extracorporeal support which succeeds in providing adequate perfusion to the brain and other “core” vital organs. Yet another problem is that superficial structures such as the skin of the forehead and earlobes, and the tissues of the fingertips (three common sites for measuring SpO2) will cool very rapidly and disproportionately when the patient is immersed in an ice water bath. The core temperature of an index finger coverd only partially by a compact and highly conductive SpO2 sensor may be as low as 10oC within 5 minutes of the patient being placed in the portable ice bath (PIB), while the brain core temperature may still be at 37oC.[8-11] Similarly, dehydration, also commonplace in the slowly dying cryopatient, may cause erroneous readings when present during hypothermia.[12]
Leaving aside the above possible artifacts, there is the problem that in some cryopatients, while all of the blood leaving the lungs to be distributed to the body may be fully, or nearly fully saturated with oxygen, there may not be enough oxygen actually being delivered to meet the metabolic demands of the tissues. For instance, resting cardiac output in a 75 kg man is ~ 4.5 liters of blood per minute, with a typical SpO2 of 98%. Even if the SpO2 remains at 98%, if the cardiac output drops to 1.5 LPM, tissue oxygenation will not be adequate, at least not under normothermic conditions (37oC). Obviously, local cooling of tissues where the oximeter sensor is placed will reduce the oxygen consumption of those tissues dramatically, and thus decrease the amount of oxygen extraction in turn resulting in an erroneously high SpO2 value in the context of the amount or volume of delivered oxygen (DO2) being supplied to the patient’s brain (and other core organs).[9, 13]
In reality, the accuracy of pulse oximetry during CPS in cryonics patients is even more problematic because this technology, even with the most advanced instruments, is effective only when the arterial oxygen saturation (SaO2) is greater than 22% in hemodynamically stable patients (and greater than 35% in hemodynamically unstable patients); core body temperature is greater than 32oC; cardiac index is greater than 1.5 L/min per m2 and the pulse pressure is > 20 mm Hg.[14] This is unlikely to be the case in most patients presenting for Standby and Stabilization. Additionally, the regional physiological effects from induction of deep hypothermia in the digits and limbs (as well as the skin of the forehead and the tissue of the earlobes), such as hypothermia-induced increase in the mean carboxyhemoglobin concentration of the blood and damping of the pulse wave under conditions of profound regional hypothermia make data obtained using this modality suspect at best, and totally unreliable at worst.[9, 13] This is information that even an experienced emergency medicine physician may neither know, nor take into account, when evaluating data being presented in a cryonics case report.
Second, it is essential that the reader/evaluator of a cryonics case report have a meta-level understanding of the procedure. This is a hard thing to describe, and an even harder skill to acquire, because it requires an integrated understanding of the whole cryopreservation process with the underlying physiological and crybiological principles that determine and guide its course. A good analogy would be a narrative story which has a beginning, middle and an end; with lots of crucial and informative dialogue, events, and happenings that occur along the way. To extend this analogy a bit further, the plot of Romeo and Juliet was shopworn when Shakespeare took it up over 400 years ago, as are the plots of Casablanca, Brokeback Mountain and Who’s Afraid of Virginia Woolf. The devil is in the detail, in the context of the narrative and in the deep knowledge of the culture that is required to make sense of these four very different stories, all of which share the same basic narrative. Absent such knowledge, a cryonics case report will be about as comprehensible as an episode of The Simpson’s or Family Guy would be to a medieval peasant.
Establishing Objective Criteria
Thus, the first problem encountered when evaluating case reports is an almost oxymoronic one: how do you do it? In other words, what criteria should be used, not just to determine how well or poorly a given case proceeded, but also how well or poorly that case was documented. In fact, to a great extent, the character and thoroughness of the documentation will determine the extent to which the case can even be evaluated by a third party. The quantity and quality of the data collected will thus determine what can be inferred about the quality of care a given patient received.
Of course, it is possible to debate what events are of significance, and also to dispute how much significance to attach to them. In this respect, evaluating cryopatient case reports might be said to be “subjective” – since there are no indisputable outcomes from the procedure, such as resuscitation and subsequent scoring of neurological deficit following sudden cardiac arrest.
Resuscitation Research: A Sad and Telling Analogy
 In fact, the validation of different modalities in resuscitation from cardiac arrest, and the “validation” of the effectiveness of cryonics procedures, have more in common than might reasonably be expected. Since bystander and emergency medical system CPR have been in widespread use throughout the Western world for 30 years, it would seem inevitable that there would be large and robust databases of survival and neurological outcome data from communities throughout Canada, the US and Western Europe. However, no such data exist! In 2005 a metanalysis of the literature disclosed that there were data from only 35 US cities or townships (representing just 9% of the US population), who had documented and published data on survival and outcome from cardiac arrest in their communities.[15] This metanalysis demonstrated a survival rate for all treated cardiac arrests of 8%, and for patients with ventricular fibrillation the rate was 18%. If these figures are extrapolated to the US population as a whole there are ~ 13,000 Americans who survive cardiac arrest long enough to be discharged from hospital out of ~ 300,000 cases of SCA each year. That’s a staggering disconnect and such a slim database provides little to go on in terms of improving the outcome for patients who will experience SCA in the future.
In fact, the validation of different modalities in resuscitation from cardiac arrest, and the “validation” of the effectiveness of cryonics procedures, have more in common than might reasonably be expected. Since bystander and emergency medical system CPR have been in widespread use throughout the Western world for 30 years, it would seem inevitable that there would be large and robust databases of survival and neurological outcome data from communities throughout Canada, the US and Western Europe. However, no such data exist! In 2005 a metanalysis of the literature disclosed that there were data from only 35 US cities or townships (representing just 9% of the US population), who had documented and published data on survival and outcome from cardiac arrest in their communities.[15] This metanalysis demonstrated a survival rate for all treated cardiac arrests of 8%, and for patients with ventricular fibrillation the rate was 18%. If these figures are extrapolated to the US population as a whole there are ~ 13,000 Americans who survive cardiac arrest long enough to be discharged from hospital out of ~ 300,000 cases of SCA each year. That’s a staggering disconnect and such a slim database provides little to go on in terms of improving the outcome for patients who will experience SCA in the future.
The reasons why reporting of outcome is so dismal in CPR have striking overlap with the reasons why cryonics case reports are so sparse, inconsistent in quality, and not infrequently fail to disclose the really important data and conclusions to be drawn from it, or fail to make the significance of these data apparent to the reader, are as follows:
1) Most cryonics organizations do not have the appropriately knowledgeable staff to organize and interpret the data in a consistent and scientifically and clinically rigorous way.
2) There is no general industry wide agreement on what constitute meaningful data and what parameters should be consistently measured and by what means and at what intervals.
3) There are no industry wide mandates or agreed upon standards for collection of data in specific fashion using agreed upon common definitions.
4) Collection, organization, graphing and reduction of data and ultimately its incorporation into a standard narrative are time consuming and can be costly. Some cryonics organizations are barely able to afford the basics of delivering cryoprotective perfusion, and some do not offer standby and acute post-cardiac arrest stabilization.
5) There is very likely a “shame factor” wherein the cryonics organizations feel “embarrassed” or threatened by their inconsistent and not infrequently poor performance in the conduct of cases and find they are psychologically unable to broadcast such performance to the world.
All five of the above factors have been identified as significant barriers to the systematic and accurate reporting of outcomes from sudden cardiac arrest (SCA) in the US.[16]
If we briefly consider #3 above, the impact of something as simple as a failure to have a commonly agreed upon definition of “survival rates” in skewing and preventing meaningful interpretation of the data becomes apparent. In 199, King County, Washington (Seattle, and the surrounding communities) published a study documenting their experience with survival of patients following SCA. They reported a survival rate ranging from 16% to 49% depending upon what the definition of “survival” was.[16] For example, when all SCA’s from all the causes are included in survival to hospital discharge, the rate was 16%. But if only witnessed arrests due to underlying heart disease (primarily myocardial infarction) with an onset of CPR of ≥4 minutes and Advanced Cardiac Life Support within ≥8 minutes were evaluated as a subset of the data, then the survival rate increases dramatically to 49%.
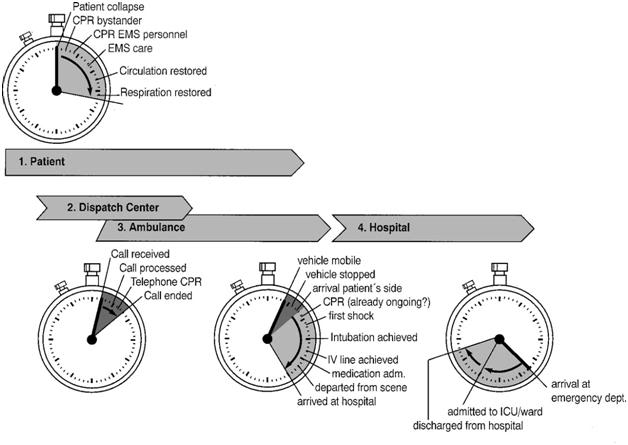 Figure 3: Different clocks used to describe event time periods and intervals during resuscitation illustrate the lack of standardization in data collection which lead to reported outcomes from cardiac arrest that are all but impossible to meaningfully interpret. Reproduced from Cummins et al.[16]
Figure 3: Different clocks used to describe event time periods and intervals during resuscitation illustrate the lack of standardization in data collection which lead to reported outcomes from cardiac arrest that are all but impossible to meaningfully interpret. Reproduced from Cummins et al.[16]
By simply changing the definition of survival, it is possible to treble the survival rate in the same community. Of course, it is equally possible to go in the opposite direction by redefining as survival as something more than simply remaining alive long enough after SCA and resuscitation to be discharged from hospital. How many of such patients were discharged to extended care facilities (ECFs) in a permanent and profoundly debilitated state due to brain damage from cerebral ischemia-reperfusion injury? How many more were able to go home and live “independently” but were too neuroinjured to return to work, or to their former level of activity and social interaction with their family and their community? Apply criteria such as, “returned to pre-arrest level of neurocognitive functioning,” or even, “returned to community capable of independent living,” and you will again radically alter the picture presented by the “survival outcome data.”
As physician and resuscitation researcher Mickey Eisenberg pointed out earlier this year:
“This is why trying to draw cross-community comparisons of (outcomes in CPR) when all parties do not agree on the definitions is like attempting to organize a tournament when each team plays by its own rules. A community, determined to be number one in cardiac arrest survival, could simply define its cases as patients with witnessed cardiac arrests in VF, who have bystander CPR, who respond to one shock with a perfusing rhythm (good blood pressure and pulse), and who wonder what’s for dinner upon arrival in the coronary care unit. Such a denominator might result in a survival rate close to 100% yet such a figure would be silly and meaningless.” http://blacklistinc.com/survive/utstein.php [17]
The Utstein Criteria
 Figure 4: Utstein Abbey in the 18th Century.
Figure 4: Utstein Abbey in the 18th Century.
This lack of uniformity of nomenclature in the resuscitation community was addressed by an international meeting held in Utstein Abbey near Stavanger, Norway in 1991. The meeting produced a detailed set of criteria with accompanying definitions, by which outcome from cardiac arrest could be uniformly measured and reported. The Utstein Criteria, established uniform and rigorous definitions, spelled out the specific data to be collected and created a template for case and group data reporting. The purpose of the Utstein Criteria was to resolve the huge discrepancies in survival after SCA across different communities and create a robust and reliable database of outcomes to facilitate improvement in resuscitation techniques.[18] In 2004 there was a further revision of the Utstein Criteria to refine definitions and further delineate the data that were deemed essential for collection. The results of this formidable, costly and now decade long effort should give heart to those who want thing to remain as they are both in cryonics and in resuscitation research; few US communities have proved willing to adopt the Utstein Criteria and reporting of outcomes from SCA remain chaotic and undecipherable.
If the conventional medical community cannot manage to impose data acquisition and reporting standards on a multibillion dollar a year, ‘life or death’ segment of the health care industry, what hope do we cryonicists have of doing anything similar? The short answer is, “None.” However, in what will likely seem an uncharacteristically optimistic statement from me, I would hasten to add that while it is impossible to impose such universal standards on cryonics organizations, it is possible to evaluate their performance and to determine, over a comparatively short periods of time, whether any meaningful change in that performance is forthcoming. If there is none, then there is a solid basis for taking actions that might previously not have been under consideration, ranging from internally lobbying for change in an accountable and calendar-driven fashion, to creating a new and more responsible organization(s) to deliver services, as an alternative to those that already exist.
End of Part I
References
1. Federowicz M, et al.,: Perfusion and freezing of a 60-year old woman. Manrise Technical Review 1973, 3(1):7-32.
2. De Wolf A: Case reports in cryonics In: Depressed Metabolism. Portland: Depressed Metabolism; 2011.
3. Neff T: Routine oximetry. A fifth vital sign? . Chest 1988 94(2):227.
4. Tierney LJ, Whooley, MA, Saint, S.: Oxygen saturation: a fifth vital sign? West J Med 1997, 166(4):285-286.
5. Thilo E, Andersen, D, Wasserstein, ML, Schmidt, J, Luckey, D.: Saturation by pulse oximetry: comparison of the results obtained by instruments of different brands. . J Pediatr 1993, 122(4):620-626.
6. Clayton D, Webb, RK, Ralston, AC, Duthie, D, Runciman, WB.: A comparison of the performance of 20 pulse oximeters under conditions of poor perfusion. Anaesthesia 1991, 46(1):3-10.
7. Gehring H, Hornberger, C, Matz, H, Konecny, E, Schmucker, P.: The effects of motion artifact and low perfusion on the performance of a new generation of pulse oximeters in volunteers undergoing hypoxemia. Respir Care 2002, 47(1):48-60.
8. Schramm W, Bartunek, A, Gilly, H.: Effect of local limb temperature on pulse oximetry and the plethysmographic pulse wave. . Int J Clin Monit Comput 1997, 14(1):17-22.
9. Nishiyama T: Pulse oximeters demonstrate different responses during hypothermia and changes in perfusion. Can J Anaesth 2006, 53(2):136-138.
10. Bergersen T, Hisdal, J, Walløe, L.: Perfusion of the human finger during cold-induced vasodilatation. Am J Physiol 1999, 276((3 Pt 2)):R731-737.
11. Chen F, Liu, ZY, Holmér, I.: Hand and finger skin temperatures in convective and contact cold exposure. . Eur J Appl Physiol Occup Physiol 1996, 72(4):372-379.
12. O’Brien C, Montain, SJ.: Hypohydration effect on finger skin temperature and blood flow during cold-water finger immersion. . J Appl Physiol 2003, 94(2):598-603.
13. Pälve H, Vuori, A.: Pulse oximetry during low cardiac output and hypothermia states immediately after open heart surgery. Crit Care Med 1989, 17(1):66-69.
14. Polanco P, Pinsky, MR.: Practical issues of hemodynamic monitoring at the bedside. Surg Clin N Am 2006, 86:1431-1456.
15. Rea T, Eisenberg, MS, Sinibaldi G, White, RD.: Incidence of EMS-treated out-of-hospital cardiac arrest in the United States. Resuscitation 2004, 63:17-24.
16. Eisenberg M, Cummins, RO, Larsen, MP.: Numerators, denominators, and survival rates: reporting survival from out-of-hospital cardiac arrest. . Am J Emerg Med 1991, 9:544-546.
17. Survive Cardiac Arrest [http://blacklistinc.com/survive/index.php]
18. Cummins R, Chamberlain, DA, Abramson, NS, et al.: Recommended guidelines for uniform reporting of data from out-of-hospital cardiac arrest: the Utstein Style. A statement for health professionals from a task force of the American Heart Association, the European Resuscitation Council, the Heart and Stroke Foundation of Canada, and the Australian Resuscitation Council. Circulation 1991, 84:960-975.
